
|
April 18, 2020 - No. 13 Deaths of Seniors During Pandemic The Need for Peoples' Empowerment • Outdated
and Unacceptable Arrangements Create - Pierre Soublière - • Deaths of Seniors in Long-Term Care and Seniors' Residences - Peggy Morton - • Workers in Seniors' Care Speak Out • Demands of the Canadian Union of Public Employees
- Eva Dance -
• Update
on Global Pandemic for Week Ending April 18 • Alberta
Government's $7.5 Billion Energy Pay-the-Rich
Scheme Deaths of Seniors During Pandemic The Need for Peoples' Empowerment in
|
|
|
Many health care workers have spoken out publicly, even when they felt their jobs were on the line, again and again addressing the measures which must be put in place.
"It is a war we are fighting and all must be protected no matter what you do. Everyone should have enough PPE [personal protective equipment] to be protected," said Abiola Tijani, who works as a personal support worker in Ottawa and is president of CUPE Local 4592, which represents personal support workers (PSWs), registered practical nurses (RPNs), housekeepers, dietary aides and others in Ottawa. On April 3, Tijani said workers were not being provided with N95 masks while working with COVID-19 patients, and fear not only getting sick themselves but that they will infect vulnerable residents. Media reports indicate that deliveries of protective equipment to long-term care homes in Ontario finally began on about April 11.
A PSW at Anson Place, a long-term care facility in Hagersville, Ontario, where 15 residents have died from COVID-19, spoke to media about the conditions in the home. Patients are still sharing rooms with as many as four other people, she said. "Their beds are two feet from each other. No wonder it is spreading," Rebecca Shaw-Piironen, told CTV News. "I don't know how much more of an emergency this could be. People are dying, and daily. I don't know what today is going to bring, or tonight. Why aren't we taking care of our people?"
Fifty-five residents have tested positive for the novel coronavirus at Anson Place as well as at least 30 staff members. This has put a massive strain on the home's ability to care for its residents, and those who are left are burnt out and overwhelmed with grief, Shaw-Piironen said.
"We need help. This is dire," she said from home as she awaited her own test results. "So many lost so fast and so many all at once. The magnitude of this... my heart just aches. Me and my coworkers, we were just so sad right now."
Shaw-Piironen said she was speaking out despite risking her job to do so. "I'd rather live in a cardboard box and feel that I did those residents right then to shut up and not say anything. She said "They need help. They're desperate. And I don't know what we have to do to get the help in there."
(With files from the Ottawa Citizen and CTV News)
Demands of the Canadian Union
of Public Employees
President of the Canadian Union of Public Employees (CUPE) Alberta Division Rory Gill sent a letter to Alberta Minister of Health Tyler Shandro on April 3 outlining necessary measures the government must take immediately at long-term care facilities. The letter called on the government to immediately implement a single-site policy for Alberta's Long-Term Care. CUPE Local 8 represents workers at McKenzie Towne where 18 residents have now died.
CUPE has called for the following principles to be followed:
- Choice: To the extent possible, workers should be able to decide in which of their current worksites to stay. In BC, this was done by allowing workers to rank their preferences of worksite.
- Job protection: when a worker is required to choose a single worksite or employer, the job at the secondary worksite should be protected. Once the emergency is over, workers should be able to return to their normal multiple shifts if they so wish, rather than finding themselves half unemployed.
- Financial stability: Work income should be maintained by ensuring that workers do not lose total hours when they commit to a single worksite (or that they are compensated for such losses). Here it is important to also consider that employers pay at different rates, which may result in lower income for workers who end up working more for the employer who pays less.
- Protection of entitlements: Workers at different facilities have different contracts, which translates into different conditions for benefits, pensions, and seniority. There should be a clear way to navigate these issues while workers who currently have two or more jobs with different employers are required to choose one.
CUPE also called on the government to put in place longer-term measures lasting at least one year. "Policies that have a good chance to succeed in creating positive incentives for workers and high-quality care for seniors include:
- Providing a wage supplement for health care workers in facilities that adopt a single-site staffing policy, similar to what is being done in BC, by standardizing wages in the sector. This will mitigate potential problems with staffing and contribute to the financial stability of workers during the emergency.
- Developing a framework for deploying workers that includes the negotiation of benefits and pensions. Employers require clear guidelines about who is responsible for financing these entitlements.
- Prohibiting employers from firing workers who choose another employer as a result of provincial restrictions on staff flows across facilities. Important steps were taken in this regard on April 2, but a more general rule is required
- Directing employers to let workers deployed with other employers to continue to accumulate seniority.
- Offering protection against loss of hours that result from provincial restrictions on movement across facilities.
Matters of Concern as the COVID-19 Pandemic Unfolds
The Queen's Speech
For only the fifth time in her 68 years as "Queen of the United Kingdom and Northern Ireland" and "Head of State of the entire British Commonwealth of Nations," on Sunday, April 5, Elizabeth II gave a special address "to the nation and to her subjects."
The media and pundits lauded it to the skies saying that, even though it was less than five minutes long, its "We're all in this together" message was very sincere and heartfelt and brought tears to their eyes.
Like her counterparts in governments which make up the Anglo-American world and community of nations under their sway, she presented the battle against the coronavirus COVID-19 as a war. In her case, it was cleverly done by evoking the 1939 British wartime song, "We'll Meet Again," as sung by the enormously popular Vera Lynn. Lynn, who is still alive at 103 years of age, was widely known as the "Forces' Sweetheart," and came to symbolise the spirit of resistance in the fight against fascism. The lyrics of the song, which Vera Lynn made famous, say:
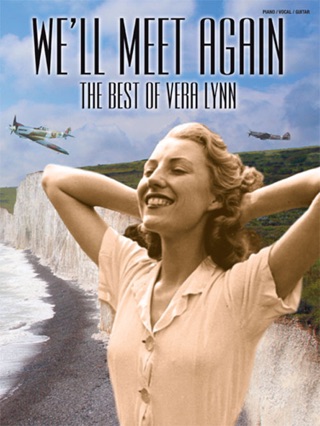 We'll meet again,
We'll meet again,
don't know where,
don't know when,
but I know we'll meet again some sunny day.
Keep smiling through
just like you always do;
'til the blue skies drive
the dark clouds far away.
So will you please say hello
to the folks that I know.
Tell them I won't be long.
They'll be happy to know
that as you saw me go
I was singing this song.
We'll meet again,
don't know where,
don't know when,
but I know we'll meet again some sunny day.
The Queen in her speech asserted: "We will succeed, and that success will belong to every one of us. We should take comfort that while we may still have much to endure, better days will return."
The context is the global pandemic and the extraordinary circumstances surrounding it, with whole societies in lock-down, people and nations isolated from each other, whilst working people are carrying out essential services at the risk of their lives. In the run-up to Sunday night's broadcast, much was made of the forthcoming speech. The BBC's Royal correspondent, Nicholas Witchell, kept appearing in mini-announcements to reveal what Her Majesty would be giving in a speech of momentous import. Parallels were drawn between this speech and the period of the Blitz in London during 1940-41 at the start of the Second World War. The reference to Vera Lynn aptly summed up the mood of the nation at the time of the Blitz and after to endure the hardships necessary to defeat fascism, whilst lifting the spirits of everyone fighting across the globe.
Whether by accident or design, no matter -- the timing of the speech coincided with the announcement that British Prime Minister Boris Johnson, already infected by the coronavirus, had been admitted into the ICU in a London hospital. The speech thus also served to rally the troops, so to speak, should anyone be worried about a power vacuum in command of the nation in time of crisis.
Since the suspension of the Parliament and declaration of emergency measures, it has become evident to all that the entire authority and decision-making power is concentrated in the Prime Minister and Cabinet-rule. Boris Johnson tested positive for the coronavirus on March 27, sending the government and chains of command into further crisis. The media and political opposition and pundits were at sixes and sevens. The prospect that the Prime Minister was himself critically ill, all of a sudden raised the scare of who would rule in his place. This became the prime concern for the ruling circles. Besides speculation about which cabinet minister was entitled to replace him, others indulged in hand-wringing suggesting that if only Britain had a written constitution, all would be clear. Or that suspending Parliament was all well and fine but the elected representatives must be given a say.
Step in the Queen to calm the nation in what is in fact a rather desperate measure to give the impression that the government has the consent of the people to implement whatever agenda it sees fit during this pandemic. The suggestion is that this is the British way. It must be done as was done in World War II and that is that. Trust us.
It is not for nothing that in the US and Canada the current battle against the coronavirus is also rendered as a war in which, this time, we are all on the same side. The US Surgeon General declared this to be "Our Pearl Harbour, Our 9/11." Canada's Prime Minister, Justin Trudeau, has been using this war metaphor over and over to communicate the message: "We will get through this together," "We look after each other -- that is the Canadian way."
All of it raises a very pertinent question: Who is the "We" the Queen represents and others refer to? The peoples of England, Scotland, Wales and the north of Ireland? Certainly not, let alone the peoples of the "Commonwealth Nations" which she declared herself head of after her coronation some more than 60 years ago.
Right from the opening sentence of her speech, it was as if this pandemic has created a blip in the otherwise solid and constant path followed by Her Majesty's government. We were told that this was "an increasingly challenging time, a time of disruption in the life of our country," that there has been "grief for some," and "financial difficulties to many." But we will prevail.
By inference, the message was: "We're all in it together," the One Nation conception of everyone pulling together and putting aside their individual aspirations and needs to get the job done and defeat the enemy. In this case, though the Queen did not directly allude to it, is the coronavirus pandemic. Indeed, she said at one point: "Together we are tackling this disease and I want to reassure you that if we remain united and resolute, then we will overcome it."
All to say that the difficulties people are facing are not man-made by successive governments who have been paying the rich handsomely from the state treasury while the people are forced to fend for themselves. In the world of the rich, essential workers are expected to put themselves in harm's way for the greater good. We will mourn their passing and carry on... It is our duty.
What people see is something else. In contrast to the spirit of the Blitz when the conditions and authority at the time of the anti-fascist war in the 1940s were in sync, today's conditions and authority clash. We are not in this together because the authorities in command have for thirty years unleashed a vicious anti-social agenda on society which has all but destroyed the system of public health, education, transportation and the aim of society based on the motto One For All and All For One. The motto of the ruling classes today is: All for One. That's it. Let Everyone Fend for Themselves and so long as we get richer, the consequences be damned.
In this regard, the essence of the Queen's speech is an appeal to workers and people of the "British Isles" and the "Commonwealth" to entrust their fate to those who have destroyed the national health system and made the rich richer and the poor poorer. There is a subliminal message that if anyone gets sick it is their fault for somehow not social distancing properly or adequately or for who cares what reason. The lack of care for the care workers, essential workers, elderly and others is not mentioned. On the contrary, a false impression is given that the government is looking after everyone.
We have a context where of necessity people are physically isolated from each other but no mechanisms are in place to find collective solutions to problems at a time the government is only looking after number one.
The conditions as a result of the coronavirus pandemic bring out starkly that people are barred from participating in having a say in the decisions which affect their lives. It is very important that in this situation, unions and workers are speaking out and demanding the kind of protective gear and working conditions they require to do their job of caring for people while they also have a huge role in getting this virus under control.
There is a lot of diversionary discussion which juxtaposes the emergency police powers which Boris Johnson has concentrated in his hands and what it means for the Parliament to be shut down. The Parliament is said to be the only mechanism the people have to express their will via their representatives. But again, in comes the Queen to rally the troops to march on and accept that they will not be seeing many of themselves ever again but they can at least cling to the hope that they will and, in the meantime, their contribution to their loved ones is to do their duty and hope for the best.
Some would say that the Queen's sincerity would be a tad more to the point if she opened her castles to house the poor and the homeless and her warehouses, kitchens and estates to feed the working poor the system she is presiding over has created and discarded. But that too diverts from the pertinent fact that the pandemic not only poses a physical danger to all the members of society without exception but also stands as a metaphor for the paralysis of power and decision-making that has engulfed the whole society in Britain, and many societies across the world. In all respects, we have reached an impasse, the resolution of which requires the acknowledgement that the situation demands the people's empowerment because the rulers are unfit to govern.
To be in the hands of the likes of Boris Johnson, whether sick himself or in perfectly good health, is a disaster for the peoples of England, Scotland, Wales and the north of Ireland. The ruling class interests he and the successive governments before him represent, no matter what their political stripe, have caused havoc in the past thirty years, destroying the medical system, forcing everyone to fend for themselves, increasing the number of poor people and the extent of their poverty, while putting the onus on the people to sort out all the problems, including this coronavirus pandemic.
And the fact is that the Queen has presided over it all to hide from the people where the decision-making power lies. She is the stand-in for the fictitious person of state which represents the rule of the high and mighty against the rule of the alleged "mob." The Royal We is not you and I, it is not the people, her alleged subjects, those who are ruled over.
By speaking in our own name we can find out who we are and what we need and how we think we can get it. The only way forward is the one which takes account of the ensemble of human relations, and to what they are revealing which is that the people cannot afford to entrust their fate to the self-serving ruling class.

Published in Workers' Weekly, newspaper of the Revolutionary Communist Party of Britain (Marxist-Leninist), April 11, 2020.
"The Way Down Is Much Slower Than the Way Up"

Director-General of the WHO Dr. Tedros Adhanom
Ghebreyesus
As the COVID-19 pandemic continues to take its toll all over the world, in Canada and various European countries as well as the United States, talk about easing restrictions to get the economy going is beginning to dominate media reports in various ways. Along with this we get more and more disinformation to divert attention from what governments are or are not doing and the need to work together to bring this pandemic under control.
Such is the case of the announcement by U.S. president Donald Trump to cut funding to the WHO, as well as a lawsuit reported against China on the part of individuals whose own country, the United States, is very likely itself criminally negligent in dealing with the pandemic.
So too the attacks on the WHO by several MPs linked to the Conservative Party of Canada as well as Liberal Irwin Cotler and Alberta Premier Jason Kenney, who has also seen fit to defame Canada's Public Health Officer Dr. Theresa Tam, in what can surely only be seen as pathetic and possibly racist attempts to sow doubt in its integrity for purposes of covering up what they themselves are up to behind the scenes.
To help Canadians find their bearings in the situation, TML Weekly is publishing below the opening remarks of the Director-General of the WHO Dr. Tedros Adhanom Ghebreyesus at his April 13 media briefing on COVID-19, followed by his opening remarks on April 15 after the U.S. suspended its funding to the WHO..
WHO Director-General's COVID-19 Briefing April 13
Good morning, good afternoon and good evening.
Some countries and communities have now endured several weeks of social and economic restrictions.
Some countries are considering when they can lift these restrictions; others are considering whether and when to introduce them.
In both cases, these decisions must be based first and foremost on protecting human health, and guided by what we know about the virus and how it behaves.
Since the beginning, this has been an area of intense focus for WHO.
As we have said many times before, this is a new virus, and the first pandemic caused by a coronavirus.
We are all learning all the time and adjusting our strategy, based on the latest available evidence.
We can only say what we know, and we can only act on what we know.
Evidence from several countries is giving us a clearer picture about this virus, how it behaves, how to stop it and how to treat it.
We know that COVID-19 spreads fast, and we know that it is deadly - 10 times deadlier than the 2009 flu pandemic.
We know that the virus can spread more easily in crowded environments like nursing homes.
We know that early case-finding, testing, isolating caring for every case and tracing every contact is essential for stopping transmission.
We know that in some countries, cases are doubling every 3 to 4 days.
However, while COVID-19 accelerates very fast, it decelerates much more slowly.
In other words, the way down is much slower than the way up.
That means control measures must be lifted slowly, and with control. It cannot happen all at once.
Control measures can only be lifted if the right public health measures are in place, including significant capacity for contact tracing.
But while some countries are considering how to ease restrictions, others are considering whether to introduce them - especially many low- and middle-income countries in Africa, Asia and Latin America.
In countries with large poor populations, the stay-at-home orders and other restrictions used in some high-income countries may not be practical.
Many poor people, migrants and refugees are already living in overcrowded conditions with few resources and little access to health care.
How do you survive a lockdown when you depend on your daily labor to eat? News reports from around the world describe how many people are in danger of being left without access to food.
Meanwhile, schools have closed for an estimated 1.4 billion children. This has halted their education, opened some to increased risk of abuse, and deprived many children of their primary source of food.
As I have said many times, physical distancing restrictions are only part of the equation, and there are many other basic public health measures that need to be put in place.
We also call on all countries to ensure that where stay-at-home measures are used, they must not be at the expense of human rights.
Each government must assess their situation, while protecting all their citizens, and especially the most vulnerable.
To support countries in making these decisions, WHO will tomorrow be publishing its updated strategic advice.
The new strategy summarizes what we've learned and charts the way forward. It includes six criteria for countries as they consider lifting restrictions:
First, that transmission is controlled;
Second, that health system capacities are in place to detect, test, isolate and treat every case and trace every contact;
Third, that outbreak risks are minimized in special settings like health facilities and nursing homes;
Fourth, that preventive measures are in place in workplaces, schools and other places where it's essential for people to go;
Fifth, that importation risks can be managed;
And sixth, that communities are fully educated, engaged and empowered to adjust to the "new norm."
Every country should be implementing a comprehensive set of measures to slow down transmission and save lives, with the aim of reaching a steady state of low-level or no transmission.
Countries must strike a balance between measures that address the mortality caused by COVID-19, and by other diseases due to overwhelmed health systems, as well as the social economic impacts.
As the pandemic has spread, its public health and socioeconomic impacts have been profound, and have disproportionately affected the vulnerable. Many populations have already experienced a lack of access to routine, essential health services.
Our global connectedness means the risk of re-introduction and resurgence of the disease will continue.
Ultimately, the development and delivery of a safe and effective vaccine will be needed to fully interrupt transmission.
Finally, I would like to thank the United Kingdom for its generous contribution of £200 million to the global response to COVID-19.
We greatly appreciate this demonstration of global solidarity.
In an editorial last week, development ministers from the UK, Denmark, Iceland, Finland, Germany, Norway and Sweden calling on all countries to join this common endeavour.
They said that tackling this disease together is our only option.
I couldn't agree more. The way forward is solidarity: solidarity at the national level, and solidarity at the global level.
WHO Director-General's COVID-19 Briefing April
15
[...]
We regret the decision of the President of the United States to order a halt in funding to the World Health Organization.
With support from the people and government of the United States, WHO works to improve the health of many of the world's poorest and most vulnerable people.
WHO is not only fighting COVID-19. We're also working to address polio, measles, malaria, Ebola, HIV, tuberculosis, malnutrition, cancer, diabetes, mental health and many other diseases and conditions.
We also work with countries to strengthen health systems and improve access to life-saving health services.
WHO is reviewing the impact on our work of any withdrawal of U.S. funding and will work with our partners to fill any financial gaps we face and to ensure our work continues uninterrupted.
Our commitment to public health, science and to serving all the people of the world without fear or favour remains absolute.
Our mission and mandate are to work with all nations equally, without regard to the size of their populations or economies.
COVID-19 does not discriminate between rich nations and poor, large nations and small. It does not discriminate between nationalities, ethnicities or ideologies.
Neither do we. This is a time for all of us to be united in our common struggle against a common threat -- a dangerous enemy.
When we are divided, the virus exploits the cracks between us.
We are committed to serving the world's people, and to accountability for the resources with which we are entrusted.
In due course, WHO's performance in tackling this pandemic will be reviewed by WHO's Member States and the independent bodies that are in place to ensure transparency and accountability. This is part of the usual process put in place by our Member States.
No doubt, areas for improvement will be identified and there will be lessons for all of us to learn.
But for now, our focus --"my focus" -- is on stopping this virus and saving lives.
WHO is grateful to the many nations, organizations and individuals who have expressed their support and commitment to WHO in recent days, including their financial commitment.
We welcome this demonstration of global solidarity, because solidarity is the rule of the game to defeat COVID-19.
WHO is getting on with the job.
We are continuing to study this virus every moment of every day, we are learning from many countries about what works, and we are sharing that information with the world.
There are more than 1.5 million enrolments in WHO's online courses through OpenWHO.org, and we will continue to expand this platform to train many more millions so we can fight COVID effectively.
Today we launched a new course for health workers on how to put on and remove personal protective equipment.
Every day we bring together thousands of clinicians, epidemiologists, educators, researchers, lab technicians, infection prevention specialists and others to exchange knowledge on COVID-19.
Our technical guidance brings together the most up-to-date evidence for health ministers, health workers and individuals.
Yesterday I had the honour of speaking to heads of state and government from the 13 ASEAN-plus-three nations.
It was inspiring to hear their experiences, and their commitment to working together to secure a shared future.
As a result of their experience with SARS and avian influenza, these countries have put in place measures and systems that are now helping them to detect and respond to COVID-19.
We're also continuing to work with partners all over the world to accelerate research and development.
More than 90 countries have joined or have expressed interest in joining the Solidarity Trial, and more than 900 patients have now been enrolled, to evaluate the safety and efficacy of four drugs and drug combinations.
Three vaccines have already started clinical trials, more than 70 others are in development, and we're working with partners to accelerate the development, production and distribution of vaccines.
In addition to the Solidarity Trial, I am glad to say that WHO has convened groups of clinicians to look at the impact of corticosteroids and other anti-inflammatory drugs on treatment outcomes.
Specifically, we are looking at oxygen use and ventilation strategies in patients. Any intervention that reduces the need for ventilation and improves outcomes for critically ill patients is important -- especially in low-resource settings, to save lives.
Last week I announced the United Nations Supply Chain Task Force, to scale up the distribution of essential medical equipment.
Yesterday the first United Nations Solidarity Flight took off, transporting personal protective equipment, ventilators and lab supplies to many countries across Africa.
The Solidarity Flight is part of a massive effort to ship lifesaving medical supplies to 95 countries across the globe, in conjunction with the World Food Programme and other agencies including Unicef, the Global Fund, Gavi, and the United Nations Department of Operational Support, Unitaid and others.
Whether it is by land, sea or air, WHO staff are working around the clock to deliver for health workers and communities everywhere.
I would like to thank the African Union, the governments of the United Arab Emirates and Ethiopia, the Jack Ma Foundation and all our partners for their solidarity with African countries at this critical moment in history. I would like to thank President Ramaphosa and the Chairperson of the African Union Commission, Moussa Faki, for their leadership.
The Solidarity Response Fund has now generated almost US$150 million from 240,000 individuals and organizations.
This Saturday, some of the biggest names in music are coming together for the One World: Together at Home concert, to generate further funds for the Solidarity Response Fund.
But not just to raise funds, to bring the world together, because we're one world, one humanity fighting a common enemy. I thank Lady Gaga, Global Citizen and all that are collaborating to put this concert together.
We will continue to work with every country and every partner, to serve the people of the world, with a relentless commitment to science, solutions and solidarity.
Since the beginning, WHO has been fighting the pandemic with every ounce of our soul and spirit. We will continue to do that until the end. That's our commitment to the whole world."
For Your Information
Update on Global Pandemic for
Week Ending April 18
Number of Cases Worldwide
As of April 18, the worldwide statistics for COVID-19 pandemic as reported by Worldometer were:
- Total reported cases: 2,287,323. This is 526,739 more than the total reported on April 11 of 1,760,584.
- Total active cases: 1,544,017. This is 286,462 more than the number reported on April 11 of 1,257,555.
- Closed cases: 743,306. This is 233,509 more than the number reported on April 11 of 509,797.
- Deaths: 157,468. This is 55,983 more deaths than on April 11, when the toll was 101,485.
- Recovered: 585,838. This is 190,434 more recoveries than on April 11, when the number was 395,404.
There were 86,496 new cases from April 16 to 17. This compares to the one-day increase in cases from April 9 to 10 of 94,625.
The disease was present in 210 countries and territories, as was the case the week prior. Of these, 79 had less than 100 cases, as compared to April 11, when there were 83 countries with less than 100 cases.
The five countries with the highest number of cases on April 18 are noted below, accompanied by the number of cases and deaths per million population, which permit a more direct comparison between countries, as well as figures from the previous week on April 11:
USA: 715,105 (613,375 active; 63,841
recovered; 37,889 deaths)
- 2,160 cases per million; 114 deaths per million
- April 11: 521,714 (473,070 active; 28,580
recovered; 20,064 deaths) and 1,519 cases per
million population; 57 deaths per million
population
Spain: 191,726 (96,886 active; 74,797
recovered; 20,043 deaths)
- 4,101 cases per million; 429 deaths per million
- April 11: 158,273 (86,524 active; 55,668
recovered; 16,801 deaths) and 3,385 cases per
million; 344 deaths per million
Italy: 175,925 (107,771 active; 44,927
recovered; 23,227 deaths)
- 2,910 cases per million; 384 deaths per million
- April 11: 147,577 (98,273 active; 30,455
recovered; 18,849 deaths) and 3,605 cases per
million; 302 deaths per million
France: 147,969 (94,868 active; 34,420
recovered; 18,681 deaths)
- 2,267 cases per million; 286 deaths per million
- April 11: 124,869 (86,740 active; 24,932
recovered; 13,197 deaths) and 1,913 cases per
million; 202 deaths per million
Germany: 142,569 (52,764 active; 85,400
recovered; 4,405 deaths)
- 1,702 cases per million; 53 deaths per million
- April 11: 122,171 (65,522 active; 53,913
recovered; 2,736 deaths) and 1,458 cases per
million; 33 deaths per million
The U.S. remains far and away the country with the highest number of cases since achieving this dubious distinction about three weeks ago. Europe, as a whole has about half the worldwide reported cases with about 1,029,214 and overall remains the worst hit region.
Cases in Top Five Countries by Region
In Europe on April 18, the country with the fifth highest number of reported cases after the four listed above, is the UK:
UK: 114,217 (98,409 active; recovered NA;
15,464 deaths)
- 1,682 cases per million; 228 deaths per million
- April 11: 73,758 (64,465 active; 344 recovered;
8,958 deaths)
- 1,086 cases per million; 132 deaths per million
Beyond the countries with the highest number of reported cases, other statistics that show the rate of infection and death relative to population show that Belgium, a country of 11.46 million people which, as of April 18, reports 3,208 cases per million and 475 deaths per million, is also relatively hard hit. Switzerland, with 8.65 million people, is also among the European countries with the highest infection and death rates.
This week Austria became one of the first European countries to relax its coronavirus measures. News agencies report that with the number of new infections stabilizing, thousands of shops nationwide reopened their doors on April 14 following a one-month lockdown. Small businesses, as well as hardware and gardening stores, are allowed to reopen "but all shoppers are required to wear masks and maintain social distance." Shopping centres, larger stores and hairdressers are set to reopen from May 1, while restaurants and hotels could resume progressively from mid-May, Chancellor Sebastian Kurz said. Austria's modified lockdown is in place until the end of April. The number of active cases in Austria peaked on April 3 with 9,334 and as of April 17 the total number of reported cases is 14,595.
In Spain, where the number of active cases is said to have nearly plateaued, Prime Minister Pedro Sanchez on April 13 allowed some workers to return to work, with police and the Red Cross handing out face masks at train stations to commuters, news agencies report. Only a few commuters were seen using Madrid's usually busy public transport, news agencies report. "Some workers in factories and the construction industry were permitted to resume work as the Spanish government looked to restart manufacturing," they report. Retail shops and services are still required to remain closed and white-collar workers still have to work from home. "Experts warned that many companies don't have access to enough health equipment to protect employees." Shops, bars and public spaces are scheduled to stay closed until at least April 26.
In Italy, the government is said to have decided to ease restrictions -- while still requiring the same social-distancing and sanitary measures -- after it saw a decline in the number of day-to-day infections, which reached 6,557 cases on March 21 and is now at just under 3,000. The country officially is under a nationwide lockdown until May 4 but news agencies report that bookshops, stationery stores and shops selling baby clothes were allowed to reopen on a trial basis on April 14. Some regional leaders, however, have opted to keep bookstores and stationery shops closed, including the hard-hit northern regions of Lombardy and Piemonte.
In France, where the rate of daily infections has yet to peak, President Emmanuel Macron announced on April 13 that the country's lockdown would be extended until May 11, saying that "There is new hope but nothing is won at the moment [...] the epidemic is not under control." From May 11, daycares, schools, colleges and lycées will be "progressively opened" as a priority, he said. However, restaurants, cafes, hotels, museums and cultural sites must stay closed and large festivals and events may only be allowed after mid-July.
In Scandinavia, Denmark reopened daycare centres and schools for children from first to fifth grades on April 15. The number of active cases in Denmark peaked on April 10 at 3,799. The rate of new daily cases has been under 200 since April 10, down from a high of 390 on April 7.
In contrast, on April 16, Britain extended its lockdown period another three weeks until May 7. People must stay at home unless they are shopping for basic necessities, or meeting medical needs. They are allowed to exercise in public once a day, and can travel to work if they are unable to work from home.
The European Commission called on EU countries to coordinate coronavirus exit plans to avoid flareups. German Foreign Minister Heiko Maas suggested that a single smartphone app can be used across the European Union to assist member states coordinate when and how to ease coronavirus lockdown rules and ensure safer measures across the bloc.
"It's important we don't end up with a patchwork of 27 coronavirus apps and 27 data protection regimes, but coordinate as best as possible," Maas said in an interview on April 14 with Germany's Funke media group. He said such an app would help ease travel and border closures across the EU and also safeguard personal privacy.
In Eurasia on April 17:
Turkey: 78,546 (68,146 active; 8,631
recovered; 1,769 deaths)
- 931 cases per million; 21 deaths per million
- April 10: 42,282 (39,232 active; 2,142
recovered; 908 deaths) and 501 cases per million;
11 deaths per million
Russia: 32,008 (29,145 active; 2,590
recovered; 273 deaths)
- 219 cases per million; 2 deaths per million
- April 10: 11,917 (11,028 active; 795 recovered;
94 deaths) and 82 cases per million; 0.6 deaths
per million
Kazakhstan: 1,546 (1,182 active; 258
recovered; 5 deaths)
- 82 cases per million; 0.9 deaths per million
- April 10: 764 (697 active; 60 recovered; 7
deaths) and 43 cases per million; 0.5 deaths per
million
Azerbajian: 1,340 (1,064 active; 174
recovered; 66 deaths)
- 132 cases per million; 1 death per million
- April 10: 991 (822 active; 159 recovered; 10
deaths) and 98 cases per million; 1 death per
million
Armenia: 1,201 (780 active; 402 recovered;
19 deaths)
- 405 cases per million; 6 deaths per million
- April 10: 937 (776 active; 149 recovered; 12
deaths) and 316 cases per million; 4 deaths per
million
The number of cases in Turkey has risen considerably in the last week, with a total number of reported cases nearing that of Iran and China, two countries with among the highest number of cases. On April 16, Turkey reported 4,801 cases in the previous 24 hours, the second highest in the world, surpassed only by the U.S. with 5,603 in that same period.
Sinan Adiyaman, head of the Turkish Medical Association (TBB), warned that, in contrast to the Turkish Ministry of Health's claims that the infection rate is stabilizing, the scale of the outbreak remained unclear because diagnostic tests only had 55-60 per cent accuracy rates and many patients had died with COVID-19 symptoms, but had been excluded from the death toll.
"We receive information based on our members' observations from across the country that the figures for cases and deaths are far higher," Adiyaman said.
The World Health Organization (WHO) said on April 14 that outbreaks were growing in Britain and Turkey.
"In fact, the WHO prediction is more accurate for Turkey. Because it is too early to say that we have taken control yet, even though health care professionals are working devotedly," Adiyaman said.
In West Asia on April 17:
Iran: 79,494 (20,472 active; 54,064
recovered; 4,958 deaths)
- 946 cases per million; 59 deaths per million
- April 10: 68,192 (28,495 active; 35,465
recovered; 4,232 deaths) and 812 cases per
million; 50 deaths per million
Israel: 12,982 (9,705 active; 3,126
recovered; 151 deaths)
- 1,500 cases per million; 17 deaths per million
- April 10: 9,968 (8,871 active; 1,011 recovered;
86 deaths) and 1,166 cases per million; 11 deaths
per million
Saudi Arabia: 7,142 (6,006 active; 1,049
recovered; 87 deaths)
- 205 cases per million; 2 deaths per million
- April 10: 3,287 (1,663 active; 351 recovered; 25
deaths) and 105 cases per million; 1 death per
million
UAE: 5,825 (4,695 active; 1,095 recovered;
35 deaths)
- 589 cases per million; 4 deaths per million
- April 10: 2,659 (2,408 active; 239 recovered; 12
deaths) and 302 cases per million; 1 death per
million
Qatar: 4,663 cases (4,192 active; 464
recovered; 7 deaths)
- 1,619 cases per million; 2 deaths per million
- April 10: 2,376 (2,164 active; 206 recovered; 6
deaths) and 872 cases per million; 2 deaths per
million
In South Asia on April 17:
India: 13,385 (11,606 active; 1,777
recovered; 452 deaths)
- 10 cases per million; 0.3 deaths per million
- April 10: 6,725 (5,879 active; 620 recovered;
226 deaths) and 5 cases per million; 0.2 cases per
million
Pakistan: 7,025 (5,125 active; 1,765
recovered; 135 deaths)
- 32 cases per million; 0.6 deaths per million
- April 10: 6,495 (5,702 active; 727 recovered; 66
deaths) and 29 cases per million; 0.3 deaths per
million
Bangladesh: 1,838 (1,705 active; 58
recovered; 75 deaths)
- 11 cases per million; 0.5 deaths per million
- April 10: 424 (364 active; 33 recovered; 27
deaths) and 3 cases per million; 0.2 deaths per
million
Afghanistan: 906 (777 active; 99
recovered; 30 deaths)
- 23 cases per million; 0.8 deaths per million
- April 10: 521 (474 active; 32 recovered; 15
deaths) and 13 cases per million; 0.4 deaths per
million
Sri Lanka: 244 (160 active; 77; 7 deaths)
- 11 cases per million; 0.3 deaths per million
- April 10: 190 (129 active; 54 recovered; 7
deaths) and 9 cases per million; 01. deaths per
million
In Southeast Asia on April 17:
Indonesia: 5,923 (4,796 active; 607
recovered; 520 deaths)
- 22 cases per million; 2 deaths per million
- April 10: 3,293 (2,761 active; 252 recovered;
280 deaths) and 13 cases per million; 1 death per
million
Philippines: 5,878 (5,004 active; 487
recovered; 387 deaths)
- 54 cases per million; 4 deaths per million
- April 17: 4,076 (3,749 active; 124 recovered;
203 deaths) and 38 cases per million; 2 deaths per
million
Malaysia: 5,251 (2,198 active; 2,967
recovered; 86 deaths)
- 162 cases per million; 3 deaths per million
- April 10: 4,346 (2,446 active; 1,830 recovered;
70 deaths) and 134 cases per million; 2 deaths per
million
Singapore: 5,050 (4,331 active; 708
recovered; 11 deaths)
- 863 cases per million; 2 deaths per million
- April 10: 2,108 (1,444 active; 492 recovered; 7
deaths) and 360 cases per million; 1 death per
million
Thailand: 2,700 (964 active; 1,689
recovered; 47 deaths)
- 39 cases per million; 0.7 deaths per million
- April 17: 2,473 (1,427 active; 1,013 recovered;
33 deaths) and 35 cases per million; 0.5 deaths
per million
Indonesia experienced a relatively sharp increase in COVID-19 infections, surpassing the Philippines and Malaysia in the past week to now have the most cases in the region. Reuters reported that on April 17 "an Indonesian official said the number of cases could reach 106,000 by July and follows criticism that a low rate of testing has hidden the extent of the spread of the virus.
"Indonesia has accelerated testing and Achmad Yurianto, a health ministry official, said on [April 17] 42,000 tests had been performed, up about three-fold in two weeks.
"'Transmission is still occurring. This has become a national disaster,' Yurianto told a televised broadcast [...]"
NPR reports that "Indonesia, which is the world's fourth most populous country, did not confirm its first cases until March 2. Since then, cases have grown exponentially and on a daily basis, spreading to all 34 provinces across an archipelago of some 17,000 islands. Still, the first lockdown orders weren't issued until over a month later, and the restrictions only applied to the Jakarta capital region and its population of some 30 million.
"This week, President Joko Widodo expanded the restrictions to some other parts of the country. He also advised the public to stay home during the Muslim holy month of Ramadan, which starts later in April. [... An] estimated 19.5 million people traveled for the Eid al-Fitr holiday marking the end of Ramadan last year, according to Bloomberg News."
Singapore, which at the beginning of the pandemic was being lauded as a model country for containment of the outbreak, has seen a rapid increase in cases since April 10. It recorded an all-time high number of new cases on April 16 with 728, whereas the daily rate of new cases had been under 100 until April 4. The vast majority of new cases are amongst foreign workers who live in cramped and substandard living conditions. In data posted by Singapore's Ministry of Manpower in 2019, there were 1,399,600 foreign workers in the country, almost 25 per cent out of a total population of 5.7 million.
On March 22, the group Transient Workers Count Too warned that employers' practices were leaving foreign workers vulnerable to infection. The group stated:
"With COVID-19 now expected to be a danger for many more months, preparedness for various scenarios is key. One possibility is that a cluster breaks out at a foreign worker dormitory.
[...]
"Currently, foreign workers are housed 12 to 20 men per room in double-decker beds. They are transported to work on the back of lorries sitting shoulder to shoulder. Neither of these conditions conforms with social distancing.
"The risk of a new cluster among this group remains undeniable."
The group also reported that some employers impose large fines if workers do not show up for work, while others refuse to grant time off for more than one or two days for medical reasons.
The Guardian reported on April 17 that "Nine dormitories, the biggest of which holds 24,000 men, have been declared isolation units by officials, while all other buildings accommodating the city-state's 300,000 [construction] workers have been placed under effective lockdown. The restrictions, an attempt to reduce further transmission, have left the dormitories even more crowded than usual as only essential workers are permitted to leave."
Regarding living conditions, the Guardian reports that "While migrants were being served food so that they did not use shared kitchens, the quality of meals was poor and lacking in nutrition. In some cases 100 men were sharing five toilets and five showers."
Mohan Dutta, a professor at Massey University in New Zealand, who has interviewed 45 migrant workers in Singapore since the outbreak began, said many feared an outbreak was inevitable due to the conditions. "Participants told me that even up until Monday [April 13] they don't have access to soap and adequate cleaning supplies," he said.
In East Asia on April 17:
China: 82,692 (116 active; 77,944
recovered; 4,632 deaths)
- 57 cases per million; 3 deaths per million
- April 10: 81,907 (1,160 active; 77,370
recovered; 3,335 deaths) and 57 cases per million;
2 deaths per million
South Korea: 10,635 (2,576 active; 7,829
recovered; 230 deaths)
- 207 cases per million; 4 deaths per million
- April 10: 10,450 (3,125 active; 7,117 recovered;
208 deaths) and 204 cases per million; 4 deaths
per million
Japan: 9,231 (8,106 active; 935 recovered;
190 deaths)
- 73 cases per million; 2 deaths per million
- April 10: 5,530 (4,746 active; 685 recovered; 99
deaths) and 44 cases per million; 0.8 deaths per
million
Taiwan: 395 (223 active; 166 recovered; 6
deaths)
- 17 cases per million; 0.3 deaths per million
- April 10: 382 (285 active; 91 recovered; 6
deaths) and 16 cases per million; 0.3 deaths per
million
China's Hubei Province on April 17 issued a "Notice on the Correction of the Number of New Coronary Pneumonia Cases Diagnosed and the Number of Diagnosed Deaths in Wuhan" in which it reported 1,290 additional deaths that had not been previously counted and reported, bringing the total number of deaths in Wuhan from 2,579 to 3,869, an increase of 50%, as the result of a revision by the Wuhan New Coronary Pneumonia Epidemic Prevention and Control. As part of this revision, 325 additional cases in Wuhan were also added. Separately, China's National Health Commission (NHC) reported 26 new cases (and no deaths) in its daily report.
Japan is the exception to the overall trend of very limited numbers of new cases in East Asia. The number of cases in Japan nearly doubled in the past week, while Prime Minister Shinzo Abe declared a nationwide state of emergency on April 16 until at least May 6, upgraded from April 8, when a state of emergency was declared in six out of 47 prefectures. Yasutoshi Nishimura, the minister in charge of Japan's emergency measures, said expanding the state of emergency to the whole country was "necessary" before the Golden Week holidays that start in late April. These are four national holidays that fall within the space of seven days, the last of which is on May 6.
On April 17, the government announced that it will offer a cash payment of 100,000 yen (U.S.$930) to every resident. Finance Minister Taro Aso said the government hoped to start payments in May.
Deutsche Welle reported on April 15 that "Nine of Japan's 47 prefectures are close to filling all the emergency hospital beds set aside for coronavirus cases, according to national broadcaster NHK, including Tokyo, Osaka, Hyogo and Fukuoka [...].
"The city government of Osaka on [April 14] issued a plea for residents to donate waterproof coats to hospitals as health workers are running out of protective clothing, an indication that the coronavirus is spreading faster than anticipated and provoking further criticism of the central government's response. [...] Osaka Mayor Ichiro Matsui said doctors and nurses at a number of hospitals are forced to wear trash bags when they treat patients. The city has requested donations of unused raincoats and asked local manufacturers of similar clothing to step up production and sell equipment to the city at fair market rates."
In North America on April 18:
USA: 715,105 (613,375 active; 63,841
recovered; 37,889 deaths)
- 2,160 cases per million; 114 deaths per million
- April 11: 521,714 (473,070 active; 28,580
recovered; 20,064 deaths) and 1,519 cases per
million population; 57 deaths per million
population
Canada: 32,412 (20,523 active; 10,543
recovered; 1,346 deaths)
- 859 cases per million; 36 deaths per million
- April 11: 22,148 (15,566 active; 6,013
recovered; 569 deaths) and 587 cases per million;
15 deaths per million
Mexico: 6,875 (4,204 active; 2,125
recovered; 546 deaths)
- 53 cases per million; 4 deaths per million
- April 11: 3,441 (2,614 active; 633 recovered;
194 deaths) and 27 cases per million; 2 deaths per
million
Despite the terrible levels of infection and deaths in the U.S., widespread layoffs in the medical system are taking place, due to the private profit motive on which the system is based. The New York Times reported on April 3, "As hospitals across the country brace for an onslaught of coronavirus patients, doctors, nurses and other health care workers -- even in emerging hot spots -- are being furloughed, reassigned or told they must take pay cuts.
"The job cuts, which stretch from Massachusetts to Nevada, are a new and possibly urgent problem for a business-oriented health care system whose hospitals must earn revenue even in a national crisis. Hospitals large and small have canceled many elective services -- often under state government orders -- as they prepare for the virus, sending revenues plummeting.
"That has left trained health care workers sidelined, even in areas around Detroit and Washington, where infection rates are climbing, and even as hard-hit hospitals are pleading for help.
[...]
"[T]he Department of Veterans Affairs is scrambling to hire health care workers for its government-run hospitals, especially in hard-hit New Orleans and Detroit, where many staff members have fallen ill. The department moved to get a federal waiver to hire retired medical workers to beef up staff levels.
"But even as some hospitals are straining to handle the influx of coronavirus patients, empty hospital beds elsewhere carry their own burden.
[...]
"Governors in dozens of states have delivered executive orders or guidelines directing hospitals to stop non-urgent procedures and surgeries to various degrees. Last month, the United States surgeon general, Dr. Jerome M. Adams, also implored hospitals to halt elective procedures.
"That has left many health systems struggling to survive."
USA Today reported on April 2 that "By June, an estimated 60,000 family practices will close or significantly scale back, and 800,000 of their employees will be laid off, furloughed or have their hours reduced as they see a decline in business during the coronavirus pandemic, according to a HealthLandscape and American Academy of Family Physicians report released [April 2].
"That represents 43 per cent of the nearly 1.9 million people employed at family medicine offices, including receptionists, medical assistants, nurses, physicians, billing staff and janitors.
"The figure doesn't include reductions at hospitals and specialty clinics that also feel the pinch."
The Washington Post reported on April 9 that "Remaining front-line workers face longer hours, and some have seen their pay cut and benefits reduced.
"For hospitals already in bad financial shape before the outbreak, the loss of income has raised doubts about their ability to keep treating patients.
[...]
"These experiences reflect the losses across the entire health-care system given the cancellation of nonessential procedures, analysts said. A typical hospital system with 1,000 beds and the ability to perform outpatient surgeries is predicted to lose around $140 million -- half its operating revenue -- over a three-month period, the Advisory Board, a consulting firm, reported this week.
"Further complicating problems has been the need to finance the purchase of additional equipment to protect staff and prepare for coronavirus patients.
"Facilities have spent large sums to create negative air pressure rooms, so infected patients can be effectively isolated from those who have not contracted the virus. Many have also set up drive-through clinics and tent facilities, further depleting their coffers, the [Inspector General of the Department of Health and Human Services] found [in an April 3 report].
[...]
"As part of the stimulus package enacted last month, the federal government has allocated $100 billion to hospitals and some other health providers to help offset lost income, pay for the construction of temporary facilities and retrofits and to buy equipment and supplies.
"But health-care executives and analysts doubt that will be sufficient. That $100 billion pot is about equal to total hospital industry revenue per month, according to the Advisory Board. Hospitals expect to be treating COVID-19 patients for several months to come."
In Central America and the Caribbean: on April 17:
Panama: 4,016 (3,809 active; 98 recovered;
109 deaths)
- 931 cases per million; 25 deaths per million
April 10: 2,752 (2,670 active; 16 recovered; 66
deaths) and 638 cases per million; 15 deaths per
million
Dominican Republic: 3,755 (3,344 active;
215 recovered; 196 deaths)
- 346 cases per million; 18 deaths per million
- April 10: 2,620 (2,396 active; 98 recovered; 126
deaths) and 242 cases per million; 12 deaths per
million
Cuba: 862 (664 active; 171 recovered; 27
deaths)
- 76 cases per million; 2 deaths per million
April 10: 565 (498 active; 51 recovered; 15
deaths) and 50 cases per million; 1 death per
million
Costa Rica: 642 (564 active; 74 recovered;
4 deaths)
- 126 cases per million; 0.8 deaths per million
- April 10: 539 (506 active; 30 recovered; 3
deaths) and 106 cases per million; 0.6 deaths per
million
Honduras: 442 (391 active; 10 recovered;
41 deaths)
- 45 cases per million; 4 deaths per million
- April 10: 382 (352 active; 7 recovered; 23
deaths) and 39 cases per million; 2 deaths per
million
Cuba now has 21 medical brigades, comprised of some 1,200 people, assisting the local efforts of 20 countries in Europe, Africa, the Middle East and Latin America and the Caribbean fight the pandemic. At the same time the U.S. blockade continues to impact Cuba's capacity to look after the well-being of its people. The Director General of Latin America and the Caribbean of the Cuban Ministry of Foreign Relations, Eugenio Martínez Enríquez, reported in his official Twitter account that the U.S. company Vyaire Medical Inc. bought IMT Medical and Acutronic, the supplier of ventilators to Cuba, and announced the suspension of ties with Cuba, because "the corporate guideline we have today is to suspend all commercial relations with Medicuba."
The Vice President of Medicuba Luis Silva reported that Cuba tried to acquire medicine and supplies with 60 firms in the U.S. of which only two replied, including Bayer, with which an agreement was signed that could not be executed, due to the prohibition issued by the U.S. Treasury Department, with the justification that, supposedly, its licence to do so had expired.
On April 1, Cuba's Ambassador to China, Carlos Miguel Pereira, denounced that the blockade had prevented the Chinese company Alibaba from bringing humanitarian aid to Cuba to fight COVID-19. On March 22, Jack Ma, founder of Alibaba and the foundation that bears his name, announced that 2 million masks, 400,000 rapid diagnostic kits and 104 respirators would be sent, in addition to equipment such as gloves and protective suits, to 24 countries in Latin America, including Cuba. However, as Ambassador Pereira noted, the U.S. transport company declined to fulfill its contract at the last minute using the argument that the regulations that comprise the economic, commercial and financial blockade imposed against the destination country, prevented it from doing so.
Cubans have not forgotten that in 1981, a major epidemic of dengue hemorrhagic fever hit Cuba, which it attributed to U.S. biological warfare, that killed 158 people, 101 of them children. The impossibility of acquiring fumigation equipment from the United States on time caused a greater delay in controlling the disease, resulting in a significant increase in the number of cases and deaths.
The fact that the blockade continues to endanger Cuban lives, especially during a global pandemic, underscores the criminal and genocidal nature of the U.S. blockade and the urgency that it be brought to an end immediately.
To that end, the Caribbean Community (CARICOM) nations were convened by Barbados for an emergency videoconference meeting on April 15 where they called for U.S. sanctions on Venezuela and Cuba to be lifted, saying "All countries must be part of the global effort to combat COVID-19." CARICOM also condemned the U.S. decision to suspend its funding of the WHO: "It is unfortunate that the resources of the WHO are under threat, in days that demand unity in leading the fight against the pandemic."
The health situation, food security and protection of the elderly from disease in the region were also addressed. In general, "the region has responded quite well to the pandemic," the Caribbean Public Health Agency Executive Director Dr. Joy St. John said at the meeting. According to Dr. St. John, the early implementation of measures in the region helped to contain the virus. But a more coordinated approach is needed to address the next phase of the pandemic.
CARICOM will consider a proposed protocol on the reopening of borders. Once the decision is taken, all Member States will at the same time adhere to this proposal. The countries also agreed that the inter-regional transport of people and goods by air and sea will also be scrutinized, making particular reference to the operations of regional air carriers.
In South America on April 17:
Brazil: 30,891 (14,913 active; 14,026
recovered; 1,954 deaths)
- 145 cases per million; 9 deaths per million
- April 10: 18,397 (17,250 active; 173 recovered;
974 deaths) and 87 cases per million; 5 deaths per
million
Peru: 12,491 (6,097 active; 6,120
recovered; 274 deaths)
- 379 cases per million; 8 deaths per million
- April 10: 5,897 (4,159 active; 1,569 recovered;
169 deaths) and 179 cases per million; 5 deaths
per million
Chile: 8,807 (5,403 active; 3,299
recovered; 105 deaths)
- 461 cases per million; 5 deaths per million
- April 10: 6,501 (4,865 active; 1,571 recovered;
65 deaths) and 340 cases per million; 3 deaths per
million
Ecuador: 8,225 (6,984 active; 838
recovered; 403 deaths)
- 466 cases per million; 23 deaths per million
- April 10: 7,161 (4,354 active; 339 recovered;
272 deaths) and 406 cases per million; 17 deaths
per million
Colombia: 3,233 (2,539 active; 550
recovered; 144 deaths)
- 64 cases per million; 3 deaths per million
- April 10: 2,223 (1,980 active; 174 recovered; 69
deaths) and 44 cases per million; 1 death per
million
There has been a sharp increase in the number of
cases in Peru in the past week, giving it the
second highest number of cases in the region in
the past week, displacing Ecuador, where despite a
relatively small increase in the number of cases
in the past week, the number of active cases and
deaths continues to rise. Ecuador has by far the
highest rate of deaths per million in the region
at 23. This number reflects official reports that
for weeks have been widely believed to be a gross
underestimate, given the collapse of the hospital
and undertaking/funeral services in the hard-hit
port city of Guayaquil in Guayas province, with
bodies remaining for days in the homes where
people have died.
It was reported this week that in the province of
Guayas there were over 5,000 deaths that could be
related to COVID-19, given that in the first two
weeks of April government figures showed there
were 6,700 people who died in the province, far
more than the average 1,000 deaths that usually
occur during that period of time.
In refuting the official figures that continue to
be reported, the mayor of Guayaquil, Cynthia
Viteri has said that patients continue to die
without ever having been tested, and that there is
no space, time or resources to be able to do
further tests and know whether or not they died of
coronavirus. She also indicated that in March
there were 1,500 more deaths in the city than in
the same period during 2019.
Another alarming fact is that more than 70 doctors
are reported to have succumbed to the virus in
Guayas.
Under the government of Lenin Moreno Ecuador's
health care system has been subjected to draconian
funding cuts and privatization, with the country's
2019 health care budget being reduced by 36 per
cent compared to 2018. In addition the program
that received the largest "investment" in the
sector was one dedicated to a restructuring of
health care by getting rid of public employees in
the system. This privatization initiative exceeded
investments in badly needed infrastructure and
equipment maintenance, contributing to the
catastrophe being witnessed today.
As if this were not enough, the Moreno government
saw fit to pay U.S.$324 million on the country's
external debt in the midst of the pandemic rather
than investing in its debilitated health care
system to save lives.
The underreporting of cases and deaths is not
unique to Ecuador, but characterizes other
countries in the region with neo-liberal
governments, many of them brought to power in
foreign-backed coups of one type or another to
dismantle existing public services as in the case
of Brazil and Bolivia, or kept in power with
foreign backing to shore up traditional privatized
systems of health care, education and others
through corruption and force, as in Chile and
Colombia.
In many of these countries doctors and nurses have
been holding public protests over the lack of even
basic PPE and other desperately needed resources
to be able to treat their patients. In an
open letter, the Colombian Medical Federation, the
Colombian Association of Scientific Societies, the
Colombian Medical College and the Federation of
Medical Unions said they would no longer work with
Health Minister Fernando Ruiz over his mishandling
of the crisis, and urged state governors to ignore
President Ivan Duque's plan to lift the quarantine
prematurely. They also have said they will not
obey the government's labour decree forcing
doctors and nurses to work without any measures in
place to protect them, saying they would abide by
the oath they took when they graduated, but that
nobody could force them to commit suicide.
Adding to the region's problems, the Pan-American
Health Organization reports there have been over a
million cases of dengue fever, a mosquito-borne
disease that is sometimes lethal, throughout the
Americas. Most of the cases are in Brazil and
Paraguay, far surpassing the number reported for
the same period last year. Other countries
affected include Bolivia and Colombia.
In Venezuela, President Nicolás Maduro stated on April 15 that his administration aims to carry out 10 million tests for COVID-19, "with the help of the World Health Organization, the Pan American Health Organization, China, Russia, Iran, and Cuba." He added that Venezuela has carried out 250,123 tests so far and has the interim goal of performing one million tests.
On April 14, Communication Minister Jorge Rodriguez reported that Venezuela has conducted the most screening for COVID-19 in Latin America, figures which are verified by Johns Hopkins University.
As of April 17, Venezuela has 204 cases (84 active; 111 recovered; 9 deaths), with a rate of 7 cases per million and 0.3 deaths per million.
In Africa on April 17:
Egypt: 2,673 (1,881 active; 596 recovered;
196 deaths)
- 26 cases per million; 2 deaths per million
- April 10: 1,699 (1,233 active; 348 recovered;
118 deaths) and 17 cases per million; 1 death per
million
South Africa: 2,605 (1,654 active; 903
recovered; 48 deaths)
- 44 cases per million; 0.8 deaths per million
- April 10: 2,003 (1,569 active; 410 recovered; 24
deaths) and 34 cases per million; 0.4 deaths per
million
Morocco: 2,528 (2,122 active; 273
recovered; 133 deaths)
- 68 cases per million; 4 deaths per million
- April 10: 1,448 (1,168 active; 109 recovered; 97
deaths) and 39 cases per million; 3 deaths per
million
Algeria: 2,268 (1,137 active; 783
recovered; 133 deaths)
- 52 cases per million; 8 deaths per million
- April l0: 1,761 (1,100 active; 405 recovered;
256 deaths) and 40 cases per million; 6 deaths per
million
Cameroon: 996 (810 active; 164 recovered;
22 deaths)
- 38 cases per million; 0.8 deaths per million
- April 10: 820 (710 active; 54 recovered; 12
deaths) and 31 cases per million; 2 deaths per
million
As of April 17, there are 19,398 cases in Africa, roughly double the number of cases a week earlier. Egypt has overtaken South Africa with the highest number of cases in the past week,
On April 13, the African Union informed that "As part of the efforts to strengthen Africa's response and preparedness in combating the COVID-19 pandemic, the African Union Commission through the Africa Centres for Disease Control and Prevention (Africa CDC) and the United Nations Development Programme (UNDP) have jointly designed a program to support on-going efforts in Africa.
"The joint program aims to coordinate COVID-19 response to recovery efforts along with Member States, Regional Economic Communities and Regional Mechanisms (RECs/RMs) as well as Civil Society Organisations (CSOs) and Faith-based Organizations (FBOs) to ensure coordinated cooperation and communication and to adopt a holistic approach. The four joint interventions areas are:
- Regional coordination and building of
synergies;
- Socio-economic, health, governance and political
impact assessments;
- Capacity building and knowledge sharing;
- Risk communication strategies and sensitization
campaigns;
"These areas are aligned with both the Africa CDC's mandate and the continental strategy on COVID-19 preparedness and response as well as the UNDP's regional approach on response to recovery.
"Specific focus on surveillance; laboratory; counter-measures guidance; health care preparedness; risk communications and social engagement; supply-chain management continues to be led by the Africa CDC."
Africa CDC on April 14 informed that "The first United Nations 'solidarity flight' left Addis Ababa, Ethiopia, today from where it will transport vital medical cargo to all countries in Africa, where supplies are desperately needed to contain the spread of COVID-19.
"The WHO cargo was transported by the United Nations World Food Programme (WFP), and includes face shields, gloves, goggles, gowns, masks, medical aprons, and thermometers, as well as ventilators.
"The cargo also includes a large quantity of medical supplies donated by the Ethiopian Prime Minister Abiy Ahmed and Jack Ma Foundation Initiative to reverse COVID-19 in Africa. The African Union, through the Africa Centres for Disease Control and Prevention (Africa CDC) is providing technical support and coordination for the distribution of the supplies."
WHO Director-General Dr. Tedros noted that "The Solidarity Flight is part of a larger effort to ship lifesaving medical supplies to 95 countries."
The WHO cargo includes one million face masks, as well as personal protective equipment, which will be enough to protect health workers while treating more than 30,000 patients across the continent.
The WHO Africa region reports that countries' experience dealing with Ebola and Influenza is being brought to bear on the COVID-19 pandemic. It gives the example of Tanzania, and states, "Tanzania is tapping into the skills of health workers already knowledgeable in infectious disease control, established influenza sentinel surveillance system and repurposing facilities to tackle the new virus.
"When the tenth Ebola outbreak erupted in the Democratic Republic of the Congo in 2018, Tanzania trained 2,400 health workers. Training sessions initially planned for Ebola were reviewed to include COVID-19. More than 300 of them have now been retrained to join the frontline ranks of the country's COVID-19 battle.
"In regions that had been identified as being at high risk of Ebola, rapid response teams were formed and trained, and authorities identified isolation areas at specific health facilities in each district and health workers trained to manage those units and handle suspected cases. The health workers and the resources are now proving critical in COVID-19 response.
"In addition, structures such as isolation units in district health facilities set up for Ebola preparedness are now being turned into COVID-19 units. All the country's 26 regions have been instructed to designate isolation areas for potential COVID-19 infection, while health worker training in patient triage for Ebola readiness now counts among the assets in curbing the spread of the new coronavirus.
[...]
"WHO Tanzania is working with the Ministries of Health in mainland Tanzania and in Zanzibar to build the capacity of health workers on clinical care, improving infection prevention, laboratory testing and other prevention measures. A total of 182 facilities have been designated to be able to isolate and treat COVID-19 in all district councils. The government has also identified 26 regional referral facilities to be capacitated to provide critical care. Most of the referral facilities already have staff trained in advanced care for Ebola, which included critical care.
[...]
"The government has also intensified public health education, working with WHO, UNICEF, religious leaders and telecommunications firms to provide facts and debunk rumours about COVID-19."
In Oceania on April 17:
Australia: 6,523 (2,639 active; 3,819
recovered; 65 deaths)
- 256 cases per million; 3 deaths per million
- April 10: 6,328 (3,043 active; 3,141 recovered;
54 deaths) and 245 cases per million; 2 deaths per
million
New Zealand: 1,409 (582 active; 816
recovered; 11 deaths)
- 292 cases per million; 2 deaths per million
- April 10: 1,239 (921 active; 317 recovered; 1
death) and 266 cases per million; 0.4 deaths per
million
Guam: 135 (5 deaths)
- April 10: 128 (4 deaths)
French Polynesia: 55
- 196 per million
- April 10: 51 and 182 per million
New Caledonia: 18 (4 active; 14 recovered)
- April 10: 18 (17 active; 1 recovered)
(With files from Worldometers,
WHO, teleSUR, Granma, Prensa Latina, Reuters, NPR,
USA Today, Washington Post, New York Times,
Guardian, Ahval, Deutsche Welle, Africa CDC,
Prensa Latina, Colombia Reports, Brasil de Fato)
|
|
(To access articles individually click on the black headline.)
Website: www.cpcml.ca Email: editor@cpcml.ca
 The health care
workers and staff at seniors' care homes, both
public and private, have been fighting for years
for the renewal of the seniors' care system,
including adequate staffing, an end to
for-private-profit care, and wages and working
conditions commensurate with the work they do. The
people who have worked so hard to keep a broken
system cobbled together are now under pressure to
continue doing this in the conditions of the
pandemic, with disastrous results.
The health care
workers and staff at seniors' care homes, both
public and private, have been fighting for years
for the renewal of the seniors' care system,
including adequate staffing, an end to
for-private-profit care, and wages and working
conditions commensurate with the work they do. The
people who have worked so hard to keep a broken
system cobbled together are now under pressure to
continue doing this in the conditions of the
pandemic, with disastrous results. Health care workers
have always been the first line of defence for the
health and safety of the seniors in the continuing
care facilities. They are the ones who have been
dealing with the results of decades of cuts,
closures and privatization and shouldering the
anti-human factor/anti-consciousness of
governments at all levels. All across the country
they have protested and demanded proper working
conditions, which are the seniors' living
conditions. They have developed tactics to make
sure these unsafe practices are blocked. But
without the decision-making power, which is what
political power is, governments use any means they
see fit to ensure that any headway they make is
taken away.
Health care workers
have always been the first line of defence for the
health and safety of the seniors in the continuing
care facilities. They are the ones who have been
dealing with the results of decades of cuts,
closures and privatization and shouldering the
anti-human factor/anti-consciousness of
governments at all levels. All across the country
they have protested and demanded proper working
conditions, which are the seniors' living
conditions. They have developed tactics to make
sure these unsafe practices are blocked. But
without the decision-making power, which is what
political power is, governments use any means they
see fit to ensure that any headway they make is
taken away. Emergency packages
and measures are still a stop gap measure. Where
is the decision that health care is a right and
that therefore every seniors' care facility and
every person requiring care has the workers and
facilities which are appropriate to their needs at
wages which meet the Canadian standard of living?
Emergency packages
and measures are still a stop gap measure. Where
is the decision that health care is a right and
that therefore every seniors' care facility and
every person requiring care has the workers and
facilities which are appropriate to their needs at
wages which meet the Canadian standard of living?
 - The cost of
accommodation and services is rising year after
year (which is confirmed by today's costs).
- The cost of
accommodation and services is rising year after
year (which is confirmed by today's costs). With the pandemic,
the working conditions of health care workers has
plummeted. As of last week, 604 health care
workers in Quebec had been infected with the
coronavirus. One nurse in the long-term care
facility of Ste-Dorothée in Laval where 13 people
lost their lives and 115 were infected, explained
that at one point she had to care for 45 patients
20 of them suffering from COVID-19. Other
employees have had to work in spite of flu
symptoms. Workers asking for N95 masks are told
that there are no such masks in seniors' care
homes and that if they want some, they will have
to buy them. Others have asserted their right to
refuse unsafe work only to be told that
disciplinary measures would be taken against them.
Long-term care facilities have been taking care of
more and more COVID-19 cases, although they are
not equipped and do not have the same protection
as hospitals.
With the pandemic,
the working conditions of health care workers has
plummeted. As of last week, 604 health care
workers in Quebec had been infected with the
coronavirus. One nurse in the long-term care
facility of Ste-Dorothée in Laval where 13 people
lost their lives and 115 were infected, explained
that at one point she had to care for 45 patients
20 of them suffering from COVID-19. Other
employees have had to work in spite of flu
symptoms. Workers asking for N95 masks are told
that there are no such masks in seniors' care
homes and that if they want some, they will have
to buy them. Others have asserted their right to
refuse unsafe work only to be told that
disciplinary measures would be taken against them.
Long-term care facilities have been taking care of
more and more COVID-19 cases, although they are
not equipped and do not have the same protection
as hospitals. A study conducted
at the London School of Economics in Britain has
also concluded that about half of all COVID-19
deaths appear to be happening in care homes in
some European countries.
A study conducted
at the London School of Economics in Britain has
also concluded that about half of all COVID-19
deaths appear to be happening in care homes in
some European countries. Twenty-five
long-term care facilities and residences for
independent and semi-independent seniors have been
deemed critical. The number of deaths in these
centres and other facilities has not been made
public. Media reports indicate that at least three
long-term care centres have 26 deaths or more.
Most of the critical facilities are on Montreal
Island and Laval, with one each in Trois-Rivières,
Shawinigan and St-Jean-sur-Richelieu.
Twenty-five
long-term care facilities and residences for
independent and semi-independent seniors have been
deemed critical. The number of deaths in these
centres and other facilities has not been made
public. Media reports indicate that at least three
long-term care centres have 26 deaths or more.
Most of the critical facilities are on Montreal
Island and Laval, with one each in Trois-Rivières,
Shawinigan and St-Jean-sur-Richelieu. According to the
Ontario Long Term Care Association, almost half of
the homes are older and need to be redeveloped.
These homes as a rule contain four kinds of
accommodation -- private, semi-private (two
people), basic (up to four seniors in one room)
and short stay (respite). The wait list as of
February 2019 was 34,834 people, with an average
wait time of 161 days to placement.
According to the
Ontario Long Term Care Association, almost half of
the homes are older and need to be redeveloped.
These homes as a rule contain four kinds of
accommodation -- private, semi-private (two
people), basic (up to four seniors in one room)
and short stay (respite). The wait list as of
February 2019 was 34,834 people, with an average
wait time of 161 days to placement.