September 22, 2020 -
No. 63
Developments
on the Health Front in Quebec
Health Care Workers Massively Reject
Government Offer 
•
Health Professionals' Union Affirms
"We Are the Solution"
- Pierre Soublière
• The Need for
Immediate Improvements in Working Conditions
- Interview, Denis Cloutier
World
Health Organization and UNICEF
• Up-to-Date Guidelines
on School-Related Public Health Measures
Developments
on the Health Front in Quebec

Demonstration
outside Quebec National Assembly September 15, 2020
On September 17, the Interprofessional Health Care Federation
of Quebec (FIQ) which represents nearly 76,000 health care workers,
announced that delegates from the FIQ and the FIQP/Private Sector,
meeting virtually as a special national council, unanimously rejected
the Quebec government's contract offer regarding working conditions.
According to the FIQ press release, the comprehensive proposal
presented last week does not respond to the much-discussed issues
raised by the nurses, nursing assistants, respiratory therapists and
clinical perfusionists that the federation represents. "The
anger aroused by the employer's offers was unequivocal.
'Disrespectful', 'insulting' and 'despicable' were among the adjectives
used by the Federation delegates. While professionals were already
expressing their distress before the pandemic, the absence of real
measures regarding their working conditions in the current state is
nothing
more and nothing less than a total lack of respect from the government
for this workforce composed mainly of women," said Nancy
Bédard, President of the FIQ. The
Federation states that the time has more than come to move from public
relations statements in the media by the Minister of Health and Social
Services, who says he is aware of what he calls the "fragility" of the
health network, to concrete proposals at the negotiating table.
The FIQ deplores the fact that there is nothing in the
government's offer to alleviate the work overload. "There
are a set of crucial issues that revolve around this, such as safety
ratios, complete and stable work teams, and overtime, whether voluntary
or not. If this issue is not addressed head-on, the major shift needed
in the health network will not be possible," writes
Jérôme Rousseau, Vice-President and co-leader of
the negotiations. A thorny issue is the need for an
increase in the number of full-time professionals. According
to the FIQ, the government wants more health care professionals to work
full-time, but it is offering no incentives or guarantees for these
positions. The government does not want to address the problem of so
many health care professionals choosing to work part-time. Health care
professionals are doing this because the government
refuses to offer them full-time positions on a fully-staffed team, with
an adequate ratio of staff to patients, where they know their schedule
in advance, can count on being able to use their vacation and other
leave entitlements, and are not held hostage by mandatory overtime.
"A full-time position in a cage with double locked locks is
not something you want. How can we attract a new generation of
professionals and have more professionals who want to work full-time?"
writes Roberto Bomba, Treasurer and co-leader of negotiations. In
addition to their sectoral negotiations on working conditions, care
professionals are also involved in negotiations on compensation issues
including wages and the pension plan, in concert with the Alliance of
the Professional and Technical Health and Social Services Staff (APTS).
FIQ and APTS held a demonstration on September 15 in front
of the Quebec National Assembly, holding huge signs reading "We Are
Defending the Network against All Odds" and "We're Done Working
Ourselves Sick!" They firmly rejected the government's wage offer of a
five per cent increase over three years, which is basically the same
offer it made to them in May of this year.  "If anyone in
this government still had doubts about the health care professionals
and health and social services professionals and technicians truly
holding up the network, the last few months should have convinced them.
The pandemic added unbearable pressure on personnel who were already
pushed to the breaking point and without
resources. It has been almost a year since the start of negotiations
with the government. Clearly, they have still not grasped the urgency
of the situation. Their salary offer has been the same for months: a
pitiful five per cent increase over three years. For us, it is simply
unacceptable," said the APTS and FIQ Presidents Andrée
Poirier and Nancy
Bédard in a joint statement on September 15. "If anyone in
this government still had doubts about the health care professionals
and health and social services professionals and technicians truly
holding up the network, the last few months should have convinced them.
The pandemic added unbearable pressure on personnel who were already
pushed to the breaking point and without
resources. It has been almost a year since the start of negotiations
with the government. Clearly, they have still not grasped the urgency
of the situation. Their salary offer has been the same for months: a
pitiful five per cent increase over three years. For us, it is simply
unacceptable," said the APTS and FIQ Presidents Andrée
Poirier and Nancy
Bédard in a joint statement on September 15.
The
two
presidents stressed that the price currently paid by their members is
very high. For months now, family/work/personal life balance has not
existed for the personnel in the health and social service network.
"131,000 people, a vast majority of them women, work in appalling
conditions. Their physical and mental health are severely
affected. Throughout this pandemic, and despite the workload and long
hours at work, the lack of protective equipment, the mandatory overtime
and very unpredictable situations, our members once again answered the
call. They deserve the pendulum to swing fairly the other way."
The current wage demand of the two unions is
12.4 per cent over three years, which includes a 7.4 per cent wage
catch-up. "If our demand was fully deserved before the pandemic
started, it is even more justified now," both presidents said.
The APTS-FIQ Alliance points out that there is a direct
correlation between improving working conditions and attracting and
retaining staff and improving both safety and access to care and
services for the population. "The government has to
understand that everyone wins: the employees will have fairer
recognition of their work, the network will become more attractive to a
workforce that it sorely needs, and the population will be able to
count on more accessible care and services" concluded Poirier and
Bédard. 
- Pierre Soublière - 
As is the case elsewhere in Quebec, Outaouais Health
professionals are resorting to sit-ins -- which, in most cases, include
refusals to work
-- because of the lack of personnel required to care for patients in
conditions which are safe for the workers providing care to patients as
well as for the patients themselves. The
most recent incident to take place because of a staff shortage was at
the Gatineau Hospital where the intensive care unit was closed from
September 12 to 16. During this closure, two patients had to be
transported to
Montreal, one to Papineauville and another to Maniwaki. The closest
hospital in Quebec with the necessary facilities
was at least a one-hour drive from Gatineau. Similarly at the beginning
of
March, the obstetrics unit at the Shawville hospital was closed and
expectant mothers had to go to Gatineau, an hour-and-a-half drive away.
This disorganization of the health system is not only an
inconvenience but represents a real threat to the safety of both
workers and patients. It is an unthinkable situation in a modern
society, hence
the importance of getting to the heart of the problem and establishing
once and for all what is holding society back and stopping health
workers from playing
their role in terms of meeting the health needs of the population.
When the intensive care unit was shut down at the Gatineau Hospital,
the head of the Integrated Centre for Health and Social
Services for the Outaouais (CISSSO) and the minister responsible for
the Outaouais simply repeated that the unit had shut down because of
parental leave and disability leave. What he did not explain is why
there were no staff available to replace those on leave, as is normal.
On the morning
of the reopening of the intensive care unit, the Quebec Minister of
Health tweeted: "Good news ... In spite of the difficult situations in
certain regions, we continue to find solutions on the ground." To call
this playing coy would be putting it mildly. Recall that when nurses
raised the problem of a lack of personnel,
long before the onset of the pandemic, the government attacked them
precisely for revealing what was really going on "on the ground" and
even claimed that speaking publicly about their working conditions was
part of the problem because it discouraged fresh blood from coming into
the system!
With the pandemic, and in large part due to
ministerial orders, employers have had a field day in limiting summer
holidays and leaves, imposing staff transfers, changing work schedules
at the last minute, imposing different shifts, as well as other
arbitrary measures. Added to that is the fact that mandatory overtime has
become even more rampant
in conditions made all the more unbearable by COVID-19, with nurses
often being required to put in 16-hour days three days in a row. In this way,
the lack of personnel because of already unbearable conditions is made
even worse, resulting in the resignation of close to 800 nurses.
The necessity to oppose attempts by the Quebec government to
put down the health professionals' union and sow doubt as to what the
problems and solutions are has arisen in all earnest. Recently, the
Fédération de l'Âge d'Or du Québec (FADOQ),
the largest organization of seniors in Quebec, has
demanded that the Legault government stop resorting to compulsory
overtime and that the health professional/patient ratio be improved. It
refers to a recent Statistics Canada study which confirms that the
average overtime hours worked by the nursing staff has increased
dramatically in Quebec, going from a weekly average of 6.2 hours in May
2019 to 16.9 hours in May 2020. FADOQ states that "the Quebec
government must
get its head out of the sand. Working until you collapse is a problem
directly related to ratios." It insists that organizational measures
must be imposed by law so that the outcome will be a more human
relationship between health professionals and patients, making it
possible for more quality time to be spent with each patient. Such
stands are required throughout Quebec to make it clear that Quebec
workers and the population at large sides with health professionals and
all frontline and essential workers, and that further attacks on their
working conditions and on their credibility will no longer be tolerated.

- Interview, Denis Cloutier - 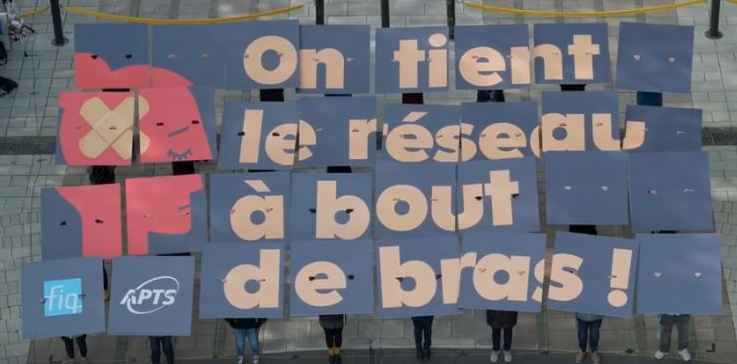
Health care workers demonstration outside Quebec National
Assembly September 15, 2020.
Denis Cloutier is the President of the Union of
Health Care Professionals of the
Est-de-l'Île-de-Montréal (FIQ SPS ESTIM).
Workers' Forum: What are
the main concerns of the union at this time regarding the conditions in
the sector? Denis Cloutier:
In the east end of Montreal, our first concern at the moment is
certainly the shortage of personnel, which is extremely severe in our
area. The pandemic has amplified the problem that was caused by years
of liberal austerity from which nurses, licensed practical nurses and
respiratory therapists have greatly
suffered. Conditions were already very difficult and the pandemic added
to the hardship. What happens in the nursing world when there is a
shortage is that the greater the staff shortage, the more hardships
there are for those who remain. The main hardship is the use of
mandatory overtime (MOT). In the east end of Montreal in particular,
several
factors, including the already existing conditions and of course
COVID-19, have led to many resignations. The pressure has increased on
those who remain, which has led to even more MOT, more mobility between
health establishments -- it's a vicious circle. We
must also understand the legacy left by the Liberal government's Minister of Health Gaétan Barrette in the way he
restructured the health care system in Quebec. The regions have been
greatly affected by the single-employer model. That is, the problems
created by the merging of institutions into Integrated Health and
Social Services
Centres (CISSS) and Integrated University Health and Social Services
Centres (CIUSSS) which became the employer for all health care
establishments in the region. Montreal is different. Minister Barrette
created several exceptions for Montreal. He created non-merged
establishments that have not been incorporated into a CISSS or a
CIUSSS. The
fact that these institutions are not merged makes them more attractive
places to work because they offer greater stability for those seeking
employment. Some of these institutions, such as the University of
Montreal Health Centre (CHUM), are beautiful, brand new hospitals that
attract staff. There is no mandatory overtime at the CHUM. There is
no residential and long-term care centre (CHSLD) attached to the CHUM,
unlike the CIUSSS and CISSS. People there work in a state-of-the-art
health care facility In the east end of Montreal,
our largest hospital is Maisonneuve-Rosemont. It's a hospital that has
had bad publicity the last few years because of a shortage of
personnel. It's an old hospital, in bad shape physically, so less
attractive. In our area there is no university. There is new real
estate development in the east end of Montreal and there
are only two hospitals, Maisonneuve-Rosemont and Santa Cabrini, while
there are several in the centre of the city. All
these changes contribute to the staff shortage which is really
worrisome. But the main reason remains the overload of work that
results in mandatory overtime. This is a phenomenon we see every day,
which creates enormous tension and suffering for the workers.

Another
of the main factors that led to the staff shortage is the use of
ministerial orders. Since the ministerial order of March 21, our
collective agreement is no longer respected. The order is still in
force in our CISSS and was used throughout the summer, during which we
had a brief respite from the pandemic. You can imagine how
much it is used when we experience a wave of infections, to
change our shifts, to send our nurses to CHSLDs to work night shifts,
evening shifts, irregular weekend shifts, without consulting them at
all. This is a serious breach of freedom for us. We
are also seeing a migration of our members to private employment
agencies. One wonders if this is not deliberately encouraged by the
government. It should be noted that with the ministerial order, the
government has broken our collective agreement, our employment
contract, but it has not broken the employment contract of the private
employment agencies. If the government was looking to promote private
agencies, it could not have done a better job. WF:
Recently, nurses have held several protest actions in workplaces.
DC: Actually, in recent
years there have been several sit-ins by nurses protesting their poor
working conditions, and these actions continue. Most recently, there
have also been actions in emergency rooms, and even in the intensive
care units, cancer clinics, etc. This typically happens when a team of
workers report for duty and
see that on the next shift five or six people are going to be missing
and therefore five or six of them will have to stay in MOT, so they
take action so that the employer will find staff for the next shift. It
can also happen that the action is organized by a team in solidarity
with the shift before them because too many of those workers have had
to
stay on MOT. These are spontaneous demonstrations of opposition to
working conditions that have become intolerable. It's a sign that
something is about to break in the network, and if we get hit by a
second wave it's certain that there will be service breakdowns.
WF: What demands are you
putting forward to change the situation? DC:
Of course there are negotiations with the government at the moment and
our situation could improve if the government agrees to our demands.
One solution that we believe will make an improvement is the
proper recognition of full-time work. There are a lot of people taking
refuge in part-time work in order to avoid the untenable conditions,
such as mandatory overtime, that are currently imposed on full-time
staff. The federation's demand is to make full-time work attractive and
start rebuilding acceptable working conditions by introducing a 12 per cent bonus
convertible into a day off every two weeks. This would involve paying a
12 per cent bonus to all employees with a full-time position or a full-time assignment. This premium could gradually be
converted into a day off in order to reach a two-week period of nine
days worked instead of 10, where full-time employees could benefit
from a minimum of two consecutive days off per week, as is the case for many people
in society. Currently full-time people work 10 days in two weeks, work
every other weekend, don't get two days off in a row in one of the
weeks, work overtime either voluntarily or under great pressure
or by outright force, are often not entitled to statutory leave. It
becomes unbearable. We see our proposal as a way to begin to establish
regular schedules to improve working conditions and attract full-time
care professionals. Full time workers must also be guaranteed their statutory vacations. To significantly reduce mandatory
overtime remains one of our main demands. All care professionals who
work part-time should have the opportunity to become full-time
employees in a stable full-time position. For us,
valuing full-time positions is a way of valuing the nurse
who is willing to commit to full-time status. We believe that it is the
beginning of a solution to end precarious working conditions in the
health care system. 
World
Health Organization and UNICEF
On September 14, the World Health Organization (WHO) and the
United Nations Children's Fund (UNICEF) issued a 10-page document
entitled "Considerations for school-related public health measures in the
context of COVID-19" that provides guidance on public health measures
related to elementary and high schools in the context of the
COVID-19 pandemic, at a time when schools in the northern hemisphere are
reopening in one form or another. It replaces a previous
document issued on May 10. It gives the following
general principles for reopening schools to prevent and minimize COVID-19 transmission: - Ensuring continuity of safe, adequate
and appropriate educational and social learning and development of
children. - Minimizing the risk of SARS-CoV-2
transmission within school and school-associated settings among
children, teachers and other school staff. -
Guarding against the potential for schools to act as amplifiers for
transmission of SARS-CoV-2 within communities. -
Ensuring school-related public health and social measures are
integrated into and support the wider measures implemented at the
community level. Among other information it
provides the following measures on prevention and control of COVID-19
transmission. Physical Distancing at School
The guidelines given for physical distancing in outdoor school
areas are to "Maintain a distance of at least one metre for both students
(all age-groups) and staff, where feasible."
Within school buildings, physical distancing
guidelines are based on the epidemiological situation in the community:
- where community-transmission is occurring, a distance of at
least one metre should be maintained between all individuals (students of
all age groups and staff) for any schools remaining open. 
Montreal
Demonstration for Safe School Reopening, August 23, 2020. (A-H Nadeau) |
-
where transmission is occurring based on clusters, the new guidelines
state that "A risk-based approach should be applied to maintain
distance of at least one metre between students. The benefits of adhering
to physical distancing of at least one metre inside a classroom should be
weighed against the social, emotional, developmental and mental
health gains from interactions between children." Teachers and support
staff "should keep at least one metre from each other and from students.
When maintaining at least one metre distance is not practical or hampers
support to students, teachers and support staff should wear a mask."
- where there are sporadic cases, it is advised that children
under the age of 12 years should not be required to keep physical
distance at all times. Where feasible, children aged 12 years and over
should keep at least one metre apart from each other. Teachers and
support staff should keep at least one metre apart from each other and
from students.
When keeping at least one metre distance is not practical or hampers
support to students, teachers and support staff should wear a mask.
- in areas where there are no cases of transmission, the
guidelines are the same as when there are sporadic cases. While
not explicitly stated, the last guideline indicates the need to err on
the side of caution and not to become complacent even if no cases have
been detected, as new cases could easily arise in the context of a
global pandemic where some people are asymptomatic carriers of COVID-19
and could cause infections to spread quickly in a school environment. Physical
Distancing Between Groups Within Schools
The WHO/UNICEF document also provides guidance on how to limit
the spread of COVID-19 between groups of students within a school. It
suggests that schools can consider:
- Limiting the mixing of classes and of age groups
for school and after-school activities. -
Alternative class modalities to limit contacts between different
classes when space and resources are limited. For example, the start
and end times of different classes can be staggered. - Modifying high school timetables, so that some students and teachers
attend school in the morning, others in the afternoon, others in the
evening. The same can be done for meal and break times. -
Increasing the number of teachers or having recourse to volunteer
support, if possible, to allow for fewer students per classroom (if
space is available). - An organized approach to
school or day-care drop off and pick up periods to ensure crowd
control, including clearly identified entry and exits, with directions
marked for foot traffic, as well as considering restrictions for
parents and caregivers entering school campus and premises. -
Educating students to not gather in large groups or in close proximity
when in lines, when leaving the school and in their free time.
Ventilation
The WHO/UNICEF guidelines state school authorities should:
- Consider using natural ventilation (i.e., opening
windows if possible and if it is safe to do so) to increase dilution of
indoor air by outdoor air when environmental conditions and building
requirements allow. - Ensure adequate ventilation
and increase total airflow supply to occupied spaces, if possible.
- If heating, ventilation and air conditioning (HVAC) systems
are used, they should be regularly inspected, maintained and cleaned.
Rigorous standards for installation and maintenance of ventilation
systems are essential to ensure that they are effective and safe. The
same applies to monitoring the condition of filters. If feasible,
increase central
air filtration to the highest level possible without significantly
diminishing design airflow. - For mechanical
systems, increase the total airflow supply and the percentage of outdoor
air, such as by using economizer modes of HVAC operations (potentially
as high as 100 per cent). First verify compatibility with HVAC system
capabilities for both temperature and humidity control as well as
compatibility with outdoor/indoor air quality
considerations. - Disable demand-control
ventilation (DCV) controls that reduce air supply based on temperature
or occupancy. - Consider running the HVAC system at
maximum outside airflow for two hours before and after times when the
building is occupied, in accordance with the manufacturer's
recommendations. Hygiene and Cleaning
Concerning hygiene and cleaning, the guidelines start by
pointing out the need to ensure all staff and students are educated
about preventative measures, COVID-19 symptoms and what to do when
feeling sick, use of masks, and the need to provide regular updates on the situation
and counter misleading information.
In terms of practical measures, the guidelines
recommend that schools: - Create a schedule for
frequent hand hygiene, especially for young children, specifically at
school arrival and at certain key moments of the school routine.
- Provide sufficient soap and clean water or alcohol-based rub
at school entrances and throughout the school and in classrooms where
feasible. - Ensure physical distancing when
students wait at hand hygiene/washing points using signage on the
ground. - Increase the frequency of regular scheduled
cleaning of the school environment, and provide custodial staff
with checklists to ensure all daily hygiene tasks, and with all
necessary cleaning and personal protective equipment. -
Assess what can be done to limit risk of exposure, or direct physical
contact in all school settings, including physical education classes,
sports, music or other physical activities and playgrounds, pools,
change rooms, science and computer labs, libraries, washrooms and dining
areas. - Provide hand hygiene stations at entrances
and exits, establish one-way circulation of athletes through sports
facilities and limit the number of persons allowed in lockers rooms
at one time; display clear information as to the number of people
allowed at the entrance of individual school facilities. -
Put in place respiratory and hand hygiene and physical distancing
measures in transportation such as school buses. Screening
and Management of Sick Students or Staff
When staff and students (and their parents) are screening
themselves as to whether they are sick and should not attend school, the
guidelines emphasize erring on the side of caution. Schools are
recommended to "Enforce the policy of 'staying at home if unwell' for
students, teachers or school staff with potential COVID-19 infection
and connect
them with local health care providers for assessment, testing and
care." To that end, it is recommended that schools provide a screening
checklist for parents/students/staff to decide whether they can go to
school, with due consideration for the local epidemiology of COVID-19.
The checklist should include: underlying medical conditions and
vulnerabilities, to protect the student/staff; recent illness or
symptoms suggestive of COVID-19, to prevent spread to others; special
circumstances in the home environment, to tailor support as needed.
The guidelines also state that the requirement for
a doctor's note to excuse absences should be waived when there is community transmission
of COVID-19. Those who have been in contact with a
COVID-19 case should go into quarantine for 14 days. In
the event of a positive COVID-19 case among students or staff, school
officials should notify
public health authorities. In such
cases there should be prompt isolation of cases and contact tracing and
quarantine of contacts should be implemented while maintaining
confidentiality, as well as decontamination of relevant areas of
schools.
Depending on the national policy, isolation of a classroom or a group
within a classroom, if contact has been limited to specific groups, can
be considered, rather than closing the entire school. Other
Information
The September 14 WHO/UNICEF document also provides information
and guidelines on the following areas:
- Communication with parents, students, teachers
and school staff
- Additional school-related measures on
re-opening a school that was closed
- Monitoring of school
operations
- Check list for assessment of school readiness
-
Research on COVID-19 in children and in schools The
document concludes by saying, "Considering that most countries are only
slowly lifting restrictions on activities and social gatherings, the
longer-term effects of keeping schools open on community transmission
are yet to be evaluated. This underscores the importance of rigorous
implementation of preventive measures when SARS-CoV-2
is circulating in the community." To see the full
10-page document, click
here. 
(To access articles individually
click on the black headline.)
PDF
PREVIOUS
ISSUES | HOME
Website:
www.cpcml.ca
Email: office@cpcml.ca | 

 "If anyone in
this government still had doubts about the health care professionals
and health and social services professionals and technicians truly
holding up the network, the last few months should have convinced them.
The pandemic added unbearable pressure on personnel who were already
pushed to the breaking point and without
resources. It has been almost a year since the start of negotiations
with the government. Clearly, they have still not grasped the urgency
of the situation. Their salary offer has been the same for months: a
pitiful five per cent increase over three years. For us, it is simply
unacceptable," said the APTS and FIQ Presidents Andrée
Poirier and Nancy
Bédard in a joint statement on September 15.
"If anyone in
this government still had doubts about the health care professionals
and health and social services professionals and technicians truly
holding up the network, the last few months should have convinced them.
The pandemic added unbearable pressure on personnel who were already
pushed to the breaking point and without
resources. It has been almost a year since the start of negotiations
with the government. Clearly, they have still not grasped the urgency
of the situation. Their salary offer has been the same for months: a
pitiful five per cent increase over three years. For us, it is simply
unacceptable," said the APTS and FIQ Presidents Andrée
Poirier and Nancy
Bédard in a joint statement on September 15.